
Musculoskeletal
Institute
Enabling Value-Based Care through patient empowerment.
The Musculoskeletal Institute at UT Health Austin is a leading innovator and practitioner of Value-Based Care, a new model of healthcare and defines success based on patient outcomes. This approach promises to revolutionize how we think about and care for patients, but the challenge lies in determining what good outcomes are.
The one voice often missing from that definition of success is the patients. Today, we make this assessment using Patient Recorded Outcomes (PROs), repetitive and technical surveys. These documents, never designed for patients, don't engender a high level of engagement, especially post-care.
This is the critical challenge today: empowering patients to be more engaged in defining the success of their care, both as a way to ensure better, more individualized outcomes while also enabling the metrics that will make Value-Based Care possible.
Working with the Musculoskeletal Institute and UT Health teams, our team identified opportunities, prototyped, and tested concepts across the patient journey for improving engagement. The outcomes from this work led to longer-term, longitudinal studies that will inform MSKI’s practices.
Design
Patient Recorded Outcomes (PROs) are the tools that make Value-Based Care possible. They could be better. To better engage patients in shaping and articulating their outcomes, we looked at two things. First, we examined the current state of patient feedback through an in-depth analysis of existing PROs, exploring how these surveys are structured and delivered. Second, we worked with the MSKI team to understand how they're using PRO metrics to shape in-clinic care and analyze post-care outcomes.
Based on that research, we worked with the MSKI team to develop dozens of concepts geared towards improving patient engagement. We mapped these concepts across the patient journey, highlighting four opportunities to explore with prototypes.
A New Tool
PROs are legacy surveys that clinicians distribute to patients in the clinic and after their care to set baselines and measure outcomes. Every single clinic at UT Health uses a different set of PROs. This reflects the needs of their clinics; it also creates a lot of redundancy and confusion for patients.
We had twos goals in our redesign, first was to standardize the structure, second was to streamline the delivery.
Make
Working with the MSKI team, we developed dozens of concepts to improve the delivery of PROs. To explore these concepts, we developed, deployed, and tested working prototypes with actual patients in MSKI’s Clinic at UT Health Austin. These prototypes reflected four-key moments in the patient journey primed for improving engagement ⇣
1. On Their Way In
As a patient, your experience begins not when you enter the clinic but at home; most doctors now ask you to fill-out forms ahead of time. This paperwork is often lengthy, repetitive, and clinically inclined. This includes PROs.
Our first priority was to improve that experience for patients. By creating a better, patient-centric design around PROs, we hoped to encourage a higher level of engagement before, during, and after care.
To test, we created a redesigned survey for select patients at MSKI’s clinic. When patients arrived for their appointment, we offered them the opportunity to try out our new version.
2. In The Clinic
Once in the clinic, we wanted to explore how education could help patients better understand their role in this new Value-Based Care model and the importance of their engagement with PROs.
To test this, we placed educational posters in each MSKI exam room explaining what Value-Based Care is, how it’s different from what they’re used to, and the importance of PROs in that care.
To evaluate the impact of our posters, we asked each participant what, if anything, they learned about value-based care in their post-visit interview.
3. On Their Way Out
As patients exit the clinic, we want to reinforce that their care does not end when they leave. As part of our prototyping, we created several behavioral nudges designed to help patients buy into this journey:
Asking patients for permission to send their follow-up PROs via text message.
Incentivizing patients to complete their post-care PROs with a $10 donation to a charity of their choice.
Providing patients reminder cards with the charity they selected and the date they’ll receive their PROs.
4. At Home
Every in-clinic intervention we created was designed to shape a better experience for patients and develop their understanding of PROs so that when they’re home, they might have a better chance at completing these critical follow-ups.
As part of our prototyping, a week after their visit, patients received a second set of interventions:
A postcard mailed to patients highlighting the charity they selected and a QR code linking them to their PROs.
A text message with a friendly note and link to complete their PROs.
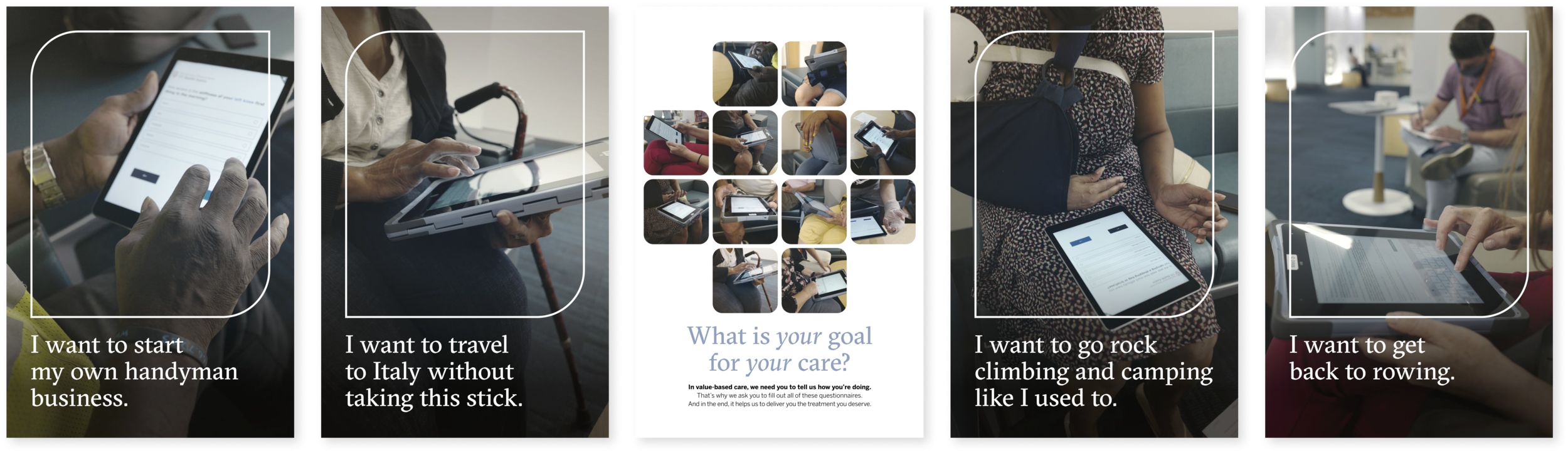
What is your goal for your care?
While testing our prototypes, we asked patients what their goals were; what they were hoping to get out of care. We heard from a retiree about wanting to drive his brand new corvette. We heard from a grandmother about wanting to play with her grandkids on the floor. We heard from a handyman about needing to get back to work.
Every single patient gave us unique, highly personal responses. Responses that can’t be captured in the existing PROs. As our models of care continue to evolve, our tools, including PRO’s, need to adapt. If you need your patients to engage with their care, you have to make room for them.
My Role
I was the project lead, managing and directing our design, prototyping, testing, and presentation. Working closely with the MSKI team, I helped steward this program into its next phase, where our partners developed our prototypes into long-term, academically rigorous research studies.
The team for this work included José Colucci , Arotin Hartounian, and Caroline Garry.
Partners














